We’ve all seen (or at least heard about) those people back in March this year who were panic-filling their trolleys with fizzy drinks and “goodies” from the snack aisles to keep the kids happy. And tonight, on Hallowe’en, the double nightmare of sugary treats and throwaway plastics sends chills down the spine. These treats are well-intentioned. Of course no-one would dream of poisoning their children intentionally or setting them up for chronic disease. But unintentionally, this is what is happening every day all over the Western world and in developing countries.

In 2016, an NHS survey estimated that 16 percent of children aged 2 to 15 in the UK were obese, and a further 12 percent were overweight. Obesity carries a high risk of type 2 diabetes, and there are currently just under four million people in the UK with the disease. Type 2 diabetes used to be called adult-onset diabetes, but that distinction no longer applies. Recent figures indicate that around 7000 children under 19 have the disease in the UK. We have a problem in this country that is brushed under the carpet to protect people’s rights and sensitivities. But in trying to protect them, we are also failing them. There is plenty of talk about the pressures on the National Health Service from obesity and related diseases. But on an individual level, what kind of help are people really getting, and is it working?
The root of problem unfortunately lies in the “help”. The NHS is creaking under the weight of the “obesity epidemic”, and all the bariatric surgery and weight-loss clinics in the world don’t seem to be making a dent in the problem. Could it be that people are getting advice from the wrong sources? If you want a document translated into Chinese, you won’t get much joy from someone who has studied linguistics. If you want to learn the violin, you’re better off going to a violinist than a general music teacher. If you have a diet-and-lifestyle-related chronic disease, your GP may have a drug for it or propose surgery, but the root cause is unlikely to be uncovered. You may find temporary relief, but if the broken soundpost inside isn’t dealt with, then the music is never going to sound right.
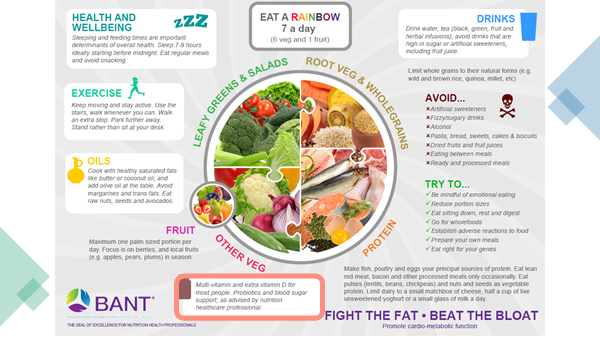
Where does the specialist start, then? There’s the rub: there is no one-size-fits-all formula. It depends on the individual. For some, it might be managing stress; for others, dealing with high levels of toxins, or rebalancing the gut microbiome. But insulin resistance will certainly be in the picture. A high-carb diet inevitably shoulders much of the blame – the same diet that has been promoted by the government for decades, with a plate that includes significant amounts of starchy carbs and processed foods. Compare the government’s “eatwell plate” with the recommended plate from BANT – the governing body in the UK for Nutritional Therapists.

What you see above is the “typical British diet”, although in fact in the average household you’ll see a lot more substances claiming to be foods on the table than are shown here. As a nation, we are the worst in Europe on that front: 50.7 percent of our calories are consumed in the form of ultra-processed food. In Italy it’s 13.4%. In Portugal, 10.2%. If the government were to promote the BANT plate and the diet and lifestyle advice around it instead of pandering to the food and pharma lobbies, we would find our beloved NHS being able to focus on what it does best: life-saving emergency treatment, and care of those with genetic and other unavoidable conditions.
Even the pressures of infectious diseases would be lessened if we all ate well instead of following the “eatwell” plate, as our immune systems would have the nutrients they need to deal with incoming pathogens. The official messages barely mention our own innate and learned defenses, although it is generally accepted that those with high blood sugar levels, heart disease and type 2 diabetes are far higher at risk from infection.
Functional medicine, and nutritional therapy based on a functional approach, are all about seeing the interconnectivity of everything that’s going on in the body, looking at what happened in someone’s life that may have triggered their dis-ease, and supporting the individual to make incremental changes to their diet and lifestyle, as well as addressing imbalances and deficiencies. So, in obesity, the traditional advice is to eat a low-fat diet and fewer calories, and to exercise. But why is it that so many people trying to follow this advice have failed over and over? For a start, focusing on calories and fat is an insult to the complex organisms we are, not to mention our rich diversity and individuality. But the main problem with this advice is that it uses fat as the scapegoat because the food industry can make money from low-fat products, as well as from sugar and refined carbohydrate products, as these are cheap to make. The tragedy for our health is that they are calorie-rich, micronutrient-poor, and addictive. They also cause insulin levels to keep on rising and rising to cope with the levels of glucose in the blood, which eventually leads to diabetes and many of our other 21st century chronic diseases.
For an in-depth look at this subject, check out this talk by David Griffiths on the Nurtural YouTube channel:





Leave A Comment